Reasons for endoscopic pituitary surgery
Endoscopic pituitary surgery is done to remove certain types of tumours that start to grow in your pituitary gland:
- Hormone-secreting tumours. These growths secrete chemical messengers that travel through the blood.
- Nonhormone-secreting tumours. These growths, (also called Non functional adenomas) are removed by surgery because as they increase in size they may cause headache and visual disturbances by compression of the optic nerve.
- Cancerous tumours. These growths may be treated with a combination of surgery, cancer drugs, and X-ray treatment.
Before endoscopic pituitary surgery
You will need to see an endocrinology specialist for an evaluation before surgery. Endocrinologists are the medical specialists that deal with glands and hormones. You will also have your vision checked before surgery. There may be need for some hormonal corrections that will need to be achieved before we can consider you fit for surgery.
Anaesthetic:
Endoscopic pituitary surgery is usually done under general anesthesia, so you will be asked to stop eating and drinking after midnight on the night before surgery. You may need to stop taking some types of medications that may increase bleeding during surgery. Don't take any over-the-counter medications before surgery without telling your doctor. You may have several blood tests, a heart rhythm test, and a chest X-ray. These will all be checked before surgery and you will need to be examined by the doctor who gives anaesthesia.
Procedure
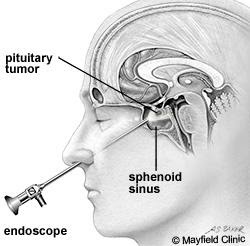
This procedure is performed to remove a pituitary tumour in the pituitary gland. The tumour is reached by working through the nose.
To accurately localise your tumour a computerised guidance system and an endoscope is used to help with the surgery. Previously these tumours were removed using the Microscope.
By working through one nostril, a hole is made at the back of the nose into the sphenoid sinus, through a layer of bone between the sphenoid sinus and the pituitary gland to gain access to the tumour.
As much of the tumour will be removed as is safe to do so.
To help fill the hole from the tumour it may be necessary to remove small pieces of fat and other tissue through a small cut in your thigh or over the abdomen.
Tissue glue may be used to secure these in place. This helps to prevent leakage of brain (cerebrospinal) fluid.
The cut in your leg/abdomen will be closed with sutures and the nose packed with a spongy material.
Risks of the procedure
Common risks include:
- CSF rhinorrhea or CSF leakage from the brain can occur through the nose after the operation. This may require further surgery. Sometimes there is a need to insert a spinal drain to reduce the pressure of the fluid within the brain. During the period of the drain being inserted, you will be restricted to the bed in a near flat position.
- Infection/Meningits. This may need antibiotics and further treatment.
- Damage to normal parts of the pituitary gland.Damage to areas of the pituitary that secrete hormones may require hormone replacement after surgery.
- Diabetes insipidus.Damage to a part of the pituitary gland that helps control urination may lead to frequent urination and thirst.
- Bleeding. A return to the operating room for further surgery may be required if bleeding occurs. Bleeding is more common if you have been taking blood thinning drugs such as Warfarin, Aspirin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin).
- Visual damage or blindness. This may be present prior to surgery and may not improve. This is due to the close proximity of the optic nerves above the pituitary gland.
Uncommon risks include:
- A heart attack because of the strain on the heart.
- Stroke or stroke like complications can occur which can cause weakness in the face, arms and legs. This could be temporary or permanent.
- Small areas of the lung may collapse, increasing the risk of chest infection. This may need antibiotics and physiotherapy.
- Increase risk in obese people of wound infection, chest infection, heart and lung complications, and thrombosis.
- Clots in the leg (deep vein thrombosis or DVT) with pain and swelling. Rarely part of this clot may break off and go into the lungs.
Rare risks include:
- Death is very rare due to this procedure.
After endoscopic surgery
You may need to stay in the hospital for 3 to 5 days. During this time, nurses will help you with any dressings and bathroom needs. You will be able to return to a normal diet as long as you are taking fluids well. You will be encouraged to get out of bed and walk as soon as you are able. While in the hospital, you will be asked to help your nurses keep track of the amount of fluids you drink and your urine output to evaluate pituitary function.
Postop - Day of surgery – you will be admitted into the ICU/HDU
- I will review you soon after surgery as will the endocrinologist when you reach the Intensive care.
- Your visual fields will be tested
- You will be nursed at a 30 degree angulation
- You will be administered oxygen via face mark
- Ice chips until fully awake and oriented.
- You will have a urinary catheter and your intake and output of fluids will be closely monitored as well as testing of the blood salts.
- You will be given 24 hours of postoperative antibiotics.
- You will need to report any fluid leakage through the nose or a sensation of salty fluid trickling down the back of the throat.
Post op Day 1.
- The antibiotics will be stopped after 24 hours.
- Hormone replacements will be charted as required.
- You will be given steam nebuliser via a face make every four hours.
- The urinary catheter will be left in place usually.
- To avoid blowing nose or straining for the next one month.
- Can be mobilised unless otherwise instructed. If there are concerns of a CS fluid leak you may be advised to take bed rest.
Postop Day 2 to discharge
- Shower with assistance if required.
- The urinary catheter and IV line may be disconnected if there is no issue with large amounts of urine being produced (diabetes insipidus)
- Commence “Flo Sinus care” kit. You will be instructed by the nurses on its use or ENT surgeon.
- If nasal pack insitu, plan for pack removal as instructed by ENT surgeon.
- Will continue to watch for CSF leak/Diabetes Insipidus.
Discharge Preparation
- I usually review on the 6th week postop.
- Endocrine and ENT reviews usually occur within the next 2 weeks. (to be discussed with respective doctor before discharge.)
- Medication will be planned as per endocrinologists.
- No driving for 3 to 6 months.
- Avoid Physical stress for a minimum of a month.
- Not to strain or blow nose for 1 month.
Aftercare at home may include:
- Pain medication to control headaches, the most common complaint after surgery
- Restricted activities – no lifting or straining until cleared by your surgeons (approx. 6 weeks)
- Follow-up visits with your endocrinologist and surgeons
- Repeat MRI, usually after 6 weeks to 3 months
- Visual testing
It is important to let your surgeons know about:
- Any headache that doesn't go away with medication
- Nausea and vomiting
- Fever
- Bleeding from the nose
- Watery discharge from the nose
- Increased urination