A primary brain tumour has grown within the brain from cells present in the normal brain. They can arise from any cell type but most commonly arise from supporting cells (glial cells) rather than the neurones themselves. These tumours are called gliomas. There are a number of different glial cells in a normal brain, therefore, there are different types of glioma, as indicated below.
-
Cell of originTumour
-
Glial cellsGliomas
-
AstrocyteAstrocytoma
-
OligodendrocyteEpendymoma
-
NeuronesGanglioglioma
Ganglioneuroma -
Pineal cellsPineocytoma
Pineoblastoma -
Reticuloendothelial cellsPrimary cerebral lymphoma
-
Vascular cellsHaemangioblastoma
Tumours are also graded from I-IV on their rate of growth (and other features) using the World Health Organisation (WHO) system. Grade I tumours are the slowest growing (benign) and grade IV are the most fastest (malignant). Some tumours have specific names:
- Grade I astrocytoma – pilocytic astrocytoma
- Grade II astrocytoma – diffuse astrocytoma (or low grade astrocytoma)
- Grade III astrocytoma – anaplastic astrocytoma
- Grade IV astrocytoma – glioblastoma multiforme
This classification is currently in the process of being updated based on a combination of hostological and genetic features.
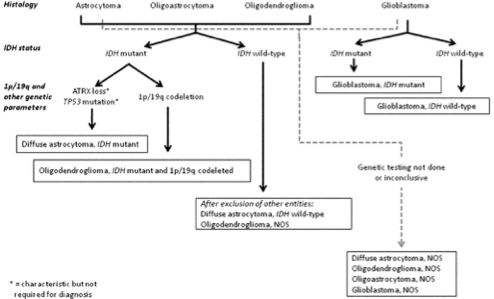
A simplified algorithm for classification of the diffuse gliomas based on histological and genetic features (see text and 2016 CNS WHO for details). A caveat to this diagram is that the diagnostic “flow” does not necessarily always proceed from histology first to molecular genetic features next, since molecular signatures can sometimes outweigh histological characteristics in achieving an “integrated” diagnosis. A similar algorithm can be followed for anaplastic- level diffuse gliomas; * Characteristic but not required for diagnosis. Reprinted from [27], with permission from the WHO
Is it a malignant tumour (cancer)? Can it be cured?
Unlike cancers elsewhere in the body, even the most rapidly growing malignant primary brain tumours do not tend to spread to other distant sites (metastasise). However, all primary brain tumours grow by infiltrating and invading the surrounding normal brain. Therefore, even if the surgeon removes what appears to be the whole tumour there will usually be small nests of tumour cells left behind amidst normal (functioning) brain tissue. Therefore it is impossible to completely cure most gliomas (grade II-IV) and patients may need other treatments, such as radiotherapy.
It is possible to cure many grade I tumours if the surgeon is able to resect (remove) the entire lesion (all the abnormal cells).
What is the best treatment for my tumour?
The best treatment for brain tumours depends on many factors including:
- Location – if the tumour lies near the surface and in a ‘safe’ area of brain your surgeon might advise an operation to remove the tumour. If an important part of the brain is involved it may not be possible to remove it safely.
- Extent – if the tumour is spreading throughout the brain diffusely it is less likely to be possible to remove it than if it is localised to one area.
- Type of tumour – some tumour types respond better to radiotherapy or chemotherapy than others.
- Grade of tumour – generally, low-grade tumours are less aggressive in the course than high grade gliomas.
- Your general health – for example there may be risks with a general anaesthetic in patients with other significant medical conditions such as heart disease.
- Age – younger patients seem to have a longer survival.
The best treatment, therefore, varies from one patient to another. For some patients there may be no need for any treatment at all. in others it may be advisable to have a combination of treatments, for example surgery, radiotherapy and chemotherapy.
Who decides on the best treatment for me?
The optimal treatment for each patient is determined by a panel of specialists. This panel ("multi-disciplinary team" - MDT) will consist of neurosurgeons (with specific expertise in brain tumours), neuro-oncologists (specialists in radiotherapy and chemotherapy for brain tumours), neuroradiologists (specialist in interpreting brain scans) and neuropathologists (make the diagnosis by examining the biopsies under the microscope). This opinion will be discussed with the patient (often a neurosurgeon initially) but ultimately, only the patient can decide which treatments he wishes to undergo.
What normally happens?
If your scan is suspicious for a primary brain tumour, your doctors will usually refer you to a neurosurgeon who will discuss your case with the MDT. You will then have a consultation with a neurosurgeon who will advise you of the treatment options. He will normally inform you of the importance of determining the precise diagnosis, which will involve an operation to take samples of the tumour and send them for analysis by a neuropathologist. This may take the form of a biopsy alone, or an operation to remove most/all of the tumour. The type and grade of the tumour will then determine your further treatment.
What is the prognosis of primary brain tumours?
The prognosis (likely outcome of treatment) depends primarily on the type and grade of the tumour. It is also influenced by age, general health, symptoms, the size and location of the tumour, and the extent of the tumour removal. Your neurosurgeon will be able to give you a more clear idea of prognosis when the final diagnosis has been made.