What is a transsphenoidal removal of pituitary tumour?
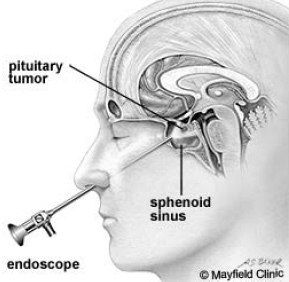
This procedure is performed to remove a pituitary tumour in the pituitary gland. The tumour is reached by working through the nose.
To accurately localise your tumour a computerised guidance system and a microscope is used to assist with the surgery.
By working through one nostril, a hole is made at the back of the nose into the sphenoid sinus, through a layer of bone between the sphenoid sinus and the pituitary gland to gain access to the tumour.
To help fill the hole from where the tumour was removed, it may be necessary to remove small pieces of fat and other tissue through a small cut in your thigh or abdomen.
Tissue glue may be used to secure the tissue fat and other tissue in place. This helps to prevent leakage of brain (cerebrospinal) fluid.
The cut in your leg will be closed with sutures and the nose packed with a spongy material.
My Anaesthetic
This procedure will require a General Anaesthetic.
See About your Anaesthetic information sheet for information about the anaesthetic and the risks involved. If you have any concerns, talk these over with your doctor.
If you have not been given an information sheet, please ask for one.
What are the risks of this specific procedure?
There are some risks/complications with this procedure.
Common risks include:
- Infection. This may need antibiotics and further treatment.
- Minor pain, bruising and/or infection from IV cannula site. This may require treatment with antibiotics.
- Bleeding. A return to the operating room for further surgery may be required if bleeding occurs. Bleeding is more common if you have been taking blood thinning drugs such as Warfarin, Aspirin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin).
- Fluid leakage from around the brain can occur after the operation. This may require further surgery.
Uncommon risks include:
- A heart attack because of the strain on the heart.
- Stroke or stroke like complications can occur which can cause weakness in the face, arms and legs. This could be temporary or permanent.
- Visual damage or blindness. This may be present prior to surgery and may not improve.
- Pituitary dysfunction. This may require further treatment.
- Small areas of the lung may collapse, increasing the risk of chest infection. This may need antibiotics and physiotherapy.
- Increase risk in obese people of wound infection, chest infection, heart and lung complications, and thrombosis.
- Clots in the leg (deep vein thrombosis or DVT) with pain and swelling. Rarely part of this clot may break off and go into the lungs.
Rare risks include:
- Death is very rare due to this procedure.