This procedure is performed to relieve pressure on the fibrous sheath which contains the spinal nerves and stabilise the spine from slipping forward any more.
X-rays will be taken during surgery to determine the correct levels of surgery.
A cut is made down the middle of the back, over the decompression site. To decompress the spine, the muscles are stripped from the bones at the back of the spine. The bones on the back of the spine (spinous process and laminae) are removed from the spine. (laminectomy)
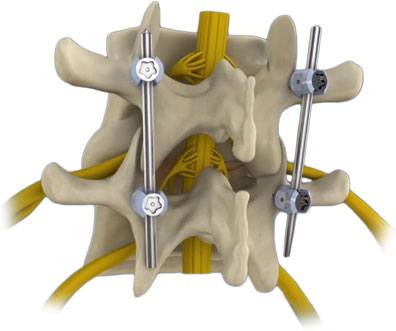
Bone and ligament is removed until the pressure is relieved from the nerves of the spine. Following the decompression, supporting screws are inserted into the pedicles of the vertebrae which require support. This is done with the aid of Computor assisted Navigation and an intraoperative CT scanner.
An intraoperative CT scan is also taken at the end of the procedure to ensure the screws are in the correct place. The screws are then joined together with a number of rods and nuts.
A separate cut may be made over the hip to harvest some hip bone.(not very frequently) Harvested bone is sometimes mixed with a bone substitute and bone growth promoting agents. It is then packed along the sides of the rods to fuse the spine.
A small plastic tube (drain) may be inserted to allow any residual fluid to be drained away. This will be removed within over the next few days depending on the amount of drainage.
The cut is closed with absorbable sutures and do not removal.
Anaesthetic
This procedure will require a General Anaesthetic.
You will be advised to fast at least 6 hours before surgery.
All blood thinners will need to be stopped for a safe period before surgery (if you have not been adviced please do ask the office for instructions.
Many essential drugs may need to be taken as per routine. Anaesthetist should advice regarding this. If they do not please contact them
What are the risks of this specific procedure?
There are some risks/complications with this procedure.
Common risks include;
- Infection. This may need antibiotics and further treatment.
- Minor pain, bruising and/or infection from IV cannula site. This may require treatment with antibiotics.
- Bleeding. If bleeding occurs further surgery may be required. Bleeding is more common if you have been taking blood thinning drugs such as Warfarin, aspirin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin).
- Small areas of the lung may collapse, increasing the risk of chest infection. This may need antibiotics and physiotherapy.
- Clots in the leg (deep vein thrombosis or DVT) with pain and swelling. Rarely part of this clot may break off and go into the lungs.
- Increase risk in obese people of wound infection, chest infection, heart and lung complications, and thrombosis.
- Pain from the bone graft site of the hip. This usually settles in time.
Uncommon risks include;
- A heart attack because of the strain on the heart.
- Stroke or stroke like complications can occur which can cause weakness in the face, arms and legs. This could be temporary or permanent.
- Nerve root injury. This may be temporary or permanent.
- Injury to the covering of the spinal cord. This may require further surgery.
- Deterioration of other discs. This may require further surgery.
- Ongoing persistent back and leg pain, with possible leg numbness due to nerve damage from compressed nerve roots. This may require further surgery.
- Leakage of cerebrospinal fluid. This may need further surgery.
- The pedicle screw may injure the nerve root. This may cause pain and/or weakness. This may be permanent.
- The metal rods or screws may break whilst the bone is healing or fusing. This may require further surgery.
- The bone may not heal or fuse. This may cause pain and require further surgery.
- Visual disturbance. This may be temporary or permanent.
Rare risks include;
- Injury to major blood vessels. This will require further urgent surgery.
- Paraplegia. This may require further surgery. This may be temporary or permanent.
- Death is very rare due to this procedure.