This surgery is performed to treat compression of the spinal cord by bony spurs that are present behind the vertebral body and not behind the discs.
The compression of the spinal cord causes Myelopathy when the patient usually complains of clumsiness and weakness of the hand and lower limbs, with varying sensory symptoms.
Surgery is then performed to relieve the pressure on the spinal cord, primarily to prevent further deterioration. Improvement is not guaranteed as recovery occurs based on how much of the damage caused by the pressure is reversible.
This surgery approaches the spine from the front. A skin crease cut is made across the side of the neck.
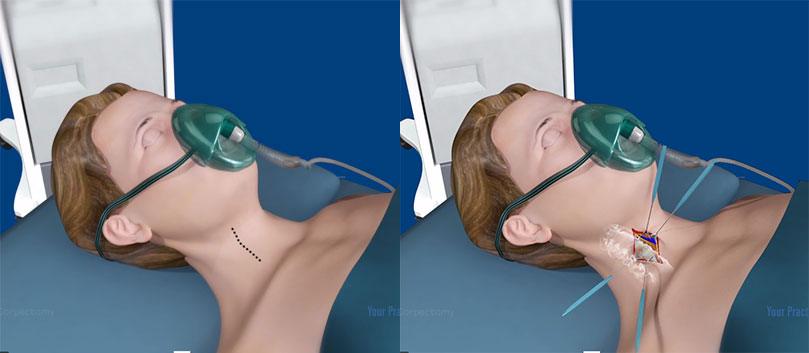
An x-ray is taken during surgery to confirm the correct level of the spine before removing the disc both above and below the involved vertebra. Using a microscope the vertebra and any bony spurs which may be compressing the nerve roots and spinal cord are also removed by drilling it out.
Once the disc is removed, the space between the neck bones is empty. To prevent the bones from collapsing and rubbing together, the space created by drilling the vertebral body is filled with an interbody cage.
The interbody cage is filled with a bone graft substitute and some of your own bone. This fuses the two neck bones together which prevents the bones rubbing together and collapsing. This is held firmly in place with a 2mm thick titanium plate and screw system.
Anaesthetic
This procedure will require a General Anaesthetic.
You will be adviced to fast at least 6 hours before surgery.
All blood thinners will need to be stopped for a safe period before surgery (if you have not been adviced please do ask the office for instructions.
Many essential drugs may need to be taken as per routine. Anaesthetist should advice regarding this. If they do not please contact them.
List of drugs that are known to cause blood thinning have to be put up.
What are the risks of this specific procedure?
There are some risks/complications with this procedure.
Common risks include:
- Infection. This may need antibiotics and further treatment.
- Minor pain, bruising and/or infection from IV cannula site. This may require treatment with antibiotics.
Uncommon risks include:
- Bleeding. A return to the operating room for further surgery may be required if bleeding occurs. Bleeding is more common if you have been taking blood thinning drugs such as Warfarin, Aspirin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin).
- A heart attack because of the strain on the heart.
- Stroke or stroke like complications can occur which can cause weakness in the face, arms and legs. This could be temporary or permanent.
- Injury to the voice box, the nerves to the voice box which causes vocal cord paralysis and a hoarse voice. This is usually temporary but may require further surgery.
- Injury to the food pipe. Most often all this results in is a difficulty is swallowing for a few days. However sometimes this may be more severe and may require further surgery.
- Injury to the carotid artery, which can cause a stroke. This may be permanent.
- Injury to the spinal cord resulting in quadriplegia. This may be temporary or permanent and may require further surgery.
- Injury to a nerve root causing a weak and numb upper limb. This may be temporary or permanent.
- Ongoing neck or upper limb pain. This may be temporary or permanent.
- Failure of fusion on the bone. This may result in pain and may require further surgery.
- Movement of the graft or inter body cage resulting in swallowing difficulties. This may require further surgery.
- Small areas of the lung may collapse, increasing the risk of chest infection. This may need antibiotics and physiotherapy.
- Increase risk in obese people of wound infection, chest infection, heart and lung complications, and thrombosis.
- Clots in the leg (deep vein thrombosis or DVT) with pain and swelling. Rarely part of this clot may break off and go into the lungs.
Rare risks include:
- Death is rare due to this procedure.
What to Expect During Your Hospital Stay?
Day of surgery
Preoperative care
- The information you have supplied in your admission pack will be confirmed by a nurse.
- The nurse will check your blood pressure, pulse, temperature, oxygen levels, medical / surgical history, and height and weight.
- A thorough limb assessment will also be carried out, and please inform the admitting nurse if you have any bowel or bladder dysfunction.
- Dependent on your age and history you will also have an ECG (Electrocardiogram) done if you have not already had one before admission.
- The nurse will check if you have had routine blood tests prior to surgery, or if you require further blood tests.
- You may be reviewed by your anaesthetist prior to your surgery.
- You will have fasted from food and fluids for at least 6 hours prior to your surgery.
- You will be measured for and given a pair of TED (anti-embolic) stockings to help reduce the risk of a blood clot post-operatively. These are to be worn before you go into theatre and are to be kept on until the day of discharge. Nursing staff will assist you to take them on and off for showering.
- You will change into a hospital gown to ensure there are no delays for theatre.
Postoperative care
- After your surgery you will remain in the recovery area until you are stable and comfortable then you will be transferred to the high dependency care unit for approximately 24 hours after your operation.
- Nursing staff will monitor your vital signs hourly. They will also monitor your wound, wound drain, intravenous drip, your oral intake and urinary output. In most cases you will have a urinary catheter insitu and this will be removed 1 -2 days after surgery.
- You are allowed to commence food and fluids as tolerated if you do not feel nauseous. You may find it painful to swallow initially but this will settle. Please advise staff if you are experiencing any increased difficulty with your swallowing or of any voice changes.
- As you will need to remain in bed, your nurse will give you a hot towel wash on returning to the ward.
- You will have oxygen delivered through nasal tubing that needs to remain in place for the first 24 hours.
- Nursing staff will ask you regularly if you have any pain and will use a pain score system to assess your level of pain.
You will be asked to rate your pain on a scale of O to 10.
O = no pain
10 = worst possible pain
Based on your answer, nursing staff will arrange appropriate pain relief medication to be given to you.
- The type of pain relief available includes tablets, injections, hot packs and less often PCA's (patient controlled analgesia) which allows you to administer your own pain relief via your drip. Note: PCA's are not routinely used and are only used if ordered by the anaesthetist.
- Please keep in mind that you may still feel some pain despite having pain relief, therefore, please inform your nurse if the medication does not reduce your pain or if your pain level increases. This may mean that your medication dose needs adjusting.
- Please advise your nurse when the pain first starts. Do not wait until the pain is bad or leave it for long periods before you take the medication as this means it will take longer to control the pain.
- If you are feeling nauseated, please let your nurse know so they can administer medications to control this and make you more comfortable
- You will be required to rest in bed initially post-operatively with head of the bed elevated to 30°. As the anaesthetic wears off you will be allowed to mobilise with assistance. Please do not attempt to mobilise without assistance.
- Pressure area care will be attended by your nurses. This involves an assisted roll in bed which will help to relieve pressure, allowing skin care to be attended.
I usually review you while you are in the recovery room and then give your designated, next of kin, a call to let them know how the surgery went and how you are after surgery. Occasionally this will not be possible due to time restraints.
Neck Bracing
For a single level anterior cervical discectomy and fusion and the Anterior cervical disc arthroplasty you will not have any postoperative neck brace.
For a 2 level Cervical discectomy or for corpectomies, you will be required to wear a Collar, when out of bed and mobilising. This brace will remain for the first 6 weeks after surgery. While wearing the brace you will not be advised to drive.
For Laminectomies with fusion, you will be required to wear the Collar for 6 weeks once again with driving restriction.
Day I
I will visit you today to discuss your operation and see how you are progressing.
Following the visit:
- Your wound drain will be usually removed after review by me.
- Your intravenous antibiotics and intravenous fluids will be ceased.
- Your wound will be inspected and monitored regularly.
- You will be commenced on a bowel regime to prevent and help avoid constipation.
- Your level of pain will be assessed to ensure you are on the appropriate medication.
- I strongly recommend you take pain relief regularly (i.e. every 4 hours) for the first 48 hours to ensure your optimal comfort and recovery. Tablets are the most frequently used type of pain management, usually given 4-6 hourly and are a step forward in your recovery towards discharge home.
- The frequency of your vital sign monitoring will be reduced.
- Your nurse will assist you with a wash as instructed. The surgical site will be kept dry and covered.
- You will continue to wear your anti-embolic stockings throughout your hospital stay. Your physiotherapist will also visit you in the morning to assess you and assist you to mobilise as tolerated.
- If your surgeon has requested that you wear a neck collar you will need to wear this when mobilising and sitting out of bed.
- We advise you to change positions regularly between lying, sitting, standing, and walking
- You may sit out of bed as tolerated depending on your level of pain.
Day 2 to discharge
- We encourage you to gradually increase your activity levels each day with the aim of increasing your independence and mobility in preparation for your discharge home.
- I will visit you daily to ensure you are progressing well and discharge planning will continue post-operatively.
- If you have any questions or concerns regarding your discharge arrangements you may contact the Clinical Nurse manager, team leader, or discharge planner in the ward at any time to discuss these. Your nurse can make this contact for you.
- Your physiotherapist will also continue to visit you daily to see how you are progressing and review your exercise and mobility regime.